Fundamentals of Inpatient Care of Surgical Patients
VBMC TRAUMA CARE SERVICES GUIDELINE
FUNDAMENTALS OF INPATIENT CARE OF SURGICAL PATIENTS
The goal of the Trauma/Acute Care Surgery service is to provide cost-effective, high-quality patient care. To achieve this goal a customer service model has been implemented. The physician/nurse team will make excellent patient care the focus of their effort. This will be accomplished by application of “best practice” models using evidence based clinical data. This will allow the physician/nurse team to direct ancillary services in the most cost-effective manner for excellent patient care.
General Guidelines for Patient Care
The
very best way to care for patients is to understand physiology and
pathophysiology. This allows the clinician to understand the treatment being
rendered. In general, if it sounds stupid, it is stupid! Remember that every
beneficial intervention also has the potential to cause harm. When a treatment
or intervention is no longer required discontinue the intervention/treatment.
Nasogastric tubes are useful for gastric decompression and to prevent emesis
associated with bowel obstruction. On the other hand, the tubes are
uncomfortable and predispose the patient to sinusitis, GERD, and aspiration.
Proton pump inhibitors and H2 antagonists reduce the incidence of stress
ulceration. However, they are associated bacterial overgrowth in the stomach
that may lead to nosocomial pneumonia. IV catheters and fluids can be lifesaving,
but they are also associated with thrombophlebitis and infection. Foley
catheters may be needed for urinary retention or monitoring of intake and
output. However, they are associated with urethral strictures and infections.
Phlebotomy for blood tests is a necessary part of patient care. However, excess
phlebotomy can and does result in anemia that can be harmful to patients.
Medications are extremely important for patient care, but drug interactions and
adverse reactions can be harmful to patients. These are a few examples of the myriads
of rather simple interventions and therapies that can and do harm patients.
Modern medical care is exceedingly expensive. Ask yourself why a particular
intervention, test, or medication is being used. Is this needed? How does this
benefit the patient? What is the harm? How much is this going to cost? What
information will I gain? Through rigorous self-examination the answer for many
of these questions is easier than you think.
Mobilization
There
is clear, irrefutable evidence that extended bed rest is harmful to patients.
Supine position and lack of mobilization leads to reductions in pulmonary
functional residual capacity, atelectasis, diminished cough, and accumulation
of dependent lung water. This makes the patient more prone to pulmonary
complications which are the most frequent cause of admission or readmission to
the ICU. Bed rest also leads to rapid loss of muscle mass leading to
de-conditioning which may increase hospital length of stay, lengthen
rehabilitation, or create the need for rehabilitation that would have not been
otherwise needed. Patients at bed rest are more prone to pressure ulcers, bowel
dysfunction, and venous thromboembolic disease.
A
primary focus of patient care should be early mobilization of the patient.
Weight-bearing status should be determined within 24 hours of admission to the
hospital and documented in the Mobility Order Set. Ambulation of the patient
should be an immediate goal, using the Mobility Plan of Care. If there are
limitations on weight-bearing these should be identified and appropriate
resources (physical therapy, equipment, etc) should be applied immediately. At
the very least, patients should be out of bed and placed in a chair in the
upright position. This does not mean bringing the bed into a sitting position
but actually getting the patients out of the bed into a chair or at least sitting
upright on the bedside. If traction or hemorrhage risk mandates bed rest, the
patients should be nursed with the head of the bed elevated at least 30
degrees. When strict logroll is in place the patient should be placed in
reverse Trendelenburg.
Mobility
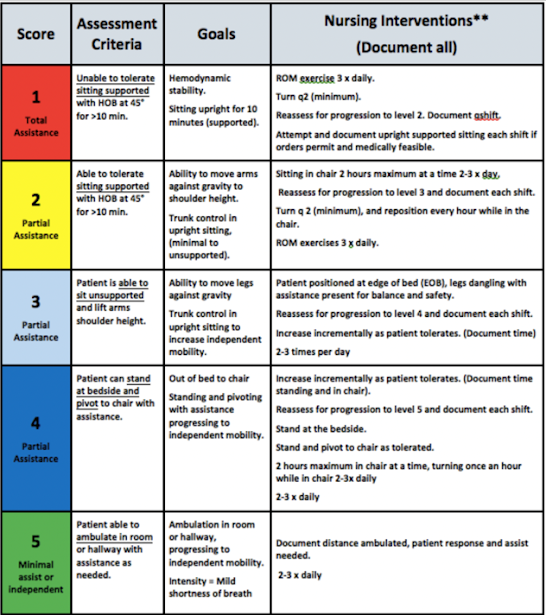
Nurse Driven Mobility Scale
Our Goal: Early progression to the patient’s best possible mobility
Please reference General Mobility and Ortho/Trauma/Spine guidelines and order set for specific instructions
Respiratory Function
Respiratory
therapy is essential for acutely ill and injured patients. Many of our patients
have co- morbid lung disease and/or a history of heavy tobacco use. Lung
function is further compromised by bed rest, obesity, chest wall trauma, pain,
surgical incisions, chest tubes, or via the use of cervical collars, back
braces, and/or traction. It is unrealistic to expect respiratory therapy
service to assume this task for most patients. Pulmonary toilet should be a
major goal for excellent nursing care.
Prevention is the key element here.
Apply
vigorous pulmonary toilet early! Use the respiratory therapist wisely. It is
far easier to prevent respiratory failure than to treat the consequences.
Patients also require education as to their role in pulmonary toilet. Patients
often equate pain with further damage. They need to understand that pulmonary
toilet may cause pain but not harm. The simplest and best pulmonary toilet is
to mobilize the patient. This requires patient effort resulting in work of
breathing that maintains respiratory muscle function. Mobilization also shifts
lung water, increases lung functional residual capacity, and reduces
atelectasis. Mobilization should be supplemented with education on maximum
voluntary ventilation, as well as coughing and deep breathing. Spirometers
(incentive spirometers, ‘blow bottles’) can and should be used to supplement
coughing and deep breathing. Some patients may require bronchodilators and/or
chest physiotherapy. Occasionally expectorants are also required. Some patients
may require nasotracheal suctioning. Pain control is essential. Patients should
be comfortable but not so somnolent that they can’t actively participate in
pulmonary toilet.
A word about supplemental oxygen
Supplemental
oxygen is expensive and unnecessary for most patients. Oxygen does not improve
respiratory failure! In fact, supplemental oxygen usually masks worsening
respiratory function that would respond to pulmonary toilet. Virtually all
human beings have arterial desaturation when recumbent or sleeping. Spot pulse
oximetry in these circumstances is of no clinical value and frequently results
in unnecessary application of supplemental oxygen. Respiratory rate and effort
combined with auscultory findings, radiograph, and subjective patient
complaints are much better determinants of respiratory failure than arterial
desaturation. In the latter circumstance, supplemental oxygen should be used
along with pulmonary toilet.
Intravenous Access
Three
quarters (75%) of all hospital bactermia events are associated with intravenous
catheters! There is a general hospital wide practice to “heparin lock” and keep
both peripheral and central venous catheters. Keeping multiple IV sites is
simply not a good practice. Every IV site represents a potential nosocomial
infection site for patients. Both insertion technique and indwell time
influence subsequent thrombophlebitis. Many catheters are placed under less-than-ideal
conditions and should be removed as soon as possible. In all but the most
unusual circumstances, a patient will require a single functioning IV access
site. Proper inspection, site care and hub cleansing should be used to maintain
function and sterility. All other intravenous access sites should be removed.